Patients
General Information about Activity Related (Sports) Injuries
Activity related injuries can be categorised into sports trauma, overuse injuries, wear and tear conditions related to activity and compression syndromes of nerve muscle or tendon. Biomechanical conditions (the way your own body shape functions in sport), training errors and age can all have an effect on the frequency, type and severity of activity related injuries.
Diagnosis, Treatments and Rehabilitation
At CSIS we take a holistic approach to the diagnosis and treatment of activity related disorders. We take into account:
Age
Adolescent athletes have greater recovery potential but also a much longer sporting career that has to be considered. More mature sports men and women may suffer with wear and tear problems that are aggravated by sports participation.
Mechanical variance
The strains on the body tissue of a 6’4” premiership goalkeeper is very different to the injuries produced in a national level martial arts athlete. Being very flexible (double jointed) can self select an athlete to achieve high standards in sports such as dancing or gymnastics. Hyperlaxity of the ligaments can of course also make the same athletes prone to joint instability with minimal trauma.
Training Errors
The frequency and rate of a training program may exploit a weakness in an athlete. Training footwear and surface conditions may create injuries such as stress fractures in an athlete without a weakness.
The recovery from sports injury is faster and more complete if the correct diagnosis is made early. Examination in the outpatient clinic by a Sports Orthopaedic Surgeon with twenty years experience as a Consultant in treating elite athletes is complimented by an array of diagnostic aides such as Ultrasound (US), Computerised Tomography (CT) and Magnetic Resonance Imaging (MRI) by radiologists respected and renowned for their expertise in the field of sports injury diagnostics.
Osteoarthritis
Anatomy of Knee Arthritis
Diagnosis
Osteoarthritis produces pain with swelling. Other symptoms include locking, catching sensations and a feeling of grinding (also called crepitus)
In the past we used to divide osteoarthritis into idiopathic (that means we don’t know why) and post-traumatic types. We now know old age is not the only cause of what was called idiopathic osteoarthritis. Genetic factors on both a cellular and morphological (how you are built) level play the major role in the development of this type of arthritis. I can highly commend the paper by Professor Michael Doherty on the subject that is available in full online. 1
The other factor that plays a powerful role in the development of premature ‘idiopathic osteoarthritis’ is the shape of the leg. Genu varus (bowed legs) and genu valgus (knocked knees) can both cause and accelerate wear changes in the inside and outside knee compartments respectively.
Natural History
Osteoarthritis is caused by the combination of biological failure of cartilage and meniscus on the one hand, and overload in one or more areas of the knee. The simple model of the knee in the erect patient has a medial and lateral compartment made up by cartilage and a medial and lateral meniscus supported by the bone of the femur and tibia. The menisci make the relatively flat surface of the tibia into a cupped or concave structure matching the convex shape of the femoral condyles.
The principle accelerator of osteoarthritis is overload. Magnitude of overload is dictated by the weight of the patient and alignment of the whole leg.
In osteoarthritis the meniscus and cartilage loose their relationship by the meniscus or the cartilage failing together or the one after the other. Once the meniscus fails it gets extruded from the joint causing all the weight bearing force to pass through either the medial (most common) or the lateral compartment producing either a varus or valgus deformity of the knee.
Cartilage is made up of:
- Cells (chondrocytes)
- Collagen
- Proteoglycan
- Water
Collagen and proteoglycan combined make up the matrix that the chondrocytes nest in. The cocooned chondrocyte is not very active and become less so as the patient gets older. The matrix behaves like steel reinforced concrete with the collagen being the ‘steel’ and the proteoglycan being the ‘concrete’.
Chondrocyte and proteoglycan quality is very similar in all patients. The big variable is the collagen. The main fibres (type II) are bound by crosslinks to their fellows by ‘lesser’ collagen molecules that are variable based on inheritance. When these ‘lesser’ collagen molecules are in short supply the main (type II) collagen structure fails. The proteoglycan, imbedded in the collagen superstructure, is extremely hydrophilic (loves water) and cannot help itself from absorbing water to the point of literally bursting. Once free fluid gets into the blistered cartilage surface he damage is relentless.
Cartilage has no ability to repair, as it has no blood supply to allow an inflammatory response to initiate the repair process. It also has no nerve supply and therefore the initial phase of damage may not be noticed. The initial breakup of cartilage does however release inflammatory and pain producing enzymes (IL1 and TNF) that causes the synovial membrane to react. When this process moves from a microscopic to macroscopic level the synovium becomes ‘sick’ causing it to loose balance between synovial fluid production and absorption. The knee now swells (develops effusion) in response to activity.
With the loss of cartilage and meniscus in either the medial or lateral knee compartment the distance between bone of the femoral condyle and tibial plateau gets less. The leg starts deforming. This results in the mechanical axis (line of force passing from hip to ankle) shifting from the middle of the knee into the compartment where the cartilage is breaking down. The process of cartilage fragmentation is thus accelerated and the forces passing to the supporting bone is increased (compartment overload).
Bone in the human body is unique in its response to load. In accordance with Volkmann’s Law it actually grows to become thicker and stiffer to resist the load increase. The circulation through this thicker bone is slower than through bone with normal density and as with most body tissue oedema ensues as water leaks from the sinusoids (vascular channels in bone). This is called bone oedema that can be clearly seen on a MRI scan. It also results in the dull gnawing rest pain of osteoarthritis.
Summary:
- Pain sources in OA are torn menisci, synovial inflammation and bone oedema.
- Joint space loss produces deformity (varus, valgus or fixed flexion) that alters the mechanical axis of the limb resulting in overload in one or more areas of the knee.
Treatment
Weight loss: Neither non-operative nor operative management of osteoarthritis will succeed in the presence of obesity. A Body Mass Index (BMI=Weight in kg/Height2) in excess of 33 will cause knee pain even in the absence of pathology. In the presence of meniscus tear or cartilage damage obesity will accelerate disease progression. Non-operative treatments will be less successful and complication rates with operative treatments will be higher.
Physiotherapy: Deformity, in the early stages, will be very minor and can be counteracted by addressing overall body posture as well as improving muscle strength and balance. Core strength and proprioception will aid in postural control. Hip abductor strength rapidly diminishes especially when joint space is lost in the medial knee compartment. The involvement of an interested and able physiotherapist is therefore crucial in the treatment of early knee arthritis.Braces and insoles: When deformity has exceeded what the patient and therapist can achieve though exercise, deformity control/correction can be achieved through external bracing or support. Physics dictate that the more remote such a brace or support is from the deformity it’s trying to correct the less effective it’ll be. Shoe insoles may therefore have a limited role to play in the very early form of the disease.
The length of the lever and surface area over which the brace is working can reduce the forces required by an external brace to control deformity. To that end I prefer to use a brace such as the Össur Unloader brace that has a good lever length and silicone thigh and calf lining over a big surface area.
Painkillers: The use of analgesia in combination with Non-Steroidal Anti-Inflammatory Drugs (NSAID’s) is fairly straightforward and algorithms for escalation by your GP are well established. The natural history of the disease will however dictate that with disease progression analgesia will become less effective. Therefore when the end stage of the disease is reached and the ‘pills don’t work anymore’, consideration is given to manage your knee arthritis with surgery.
Surgery: Arthroscopy will not help the pain of arthritis. It may have a role to play your main symptom is that of locking or catching of the knee.
The only effective surgery for arthritis is osteotomy and knee joint replacement surgery. I don’t offer knee replacement surgery as it falls out with the scope of my practice of joint reconstruction in active, younger patients with earlier stages of arthritis. Joint replacement is generally reserved for the older patient with end stage knee arthritis. It is done by most lower limb orthopaedic surgeons
Osteotomy changes leg alignment to shift the mechanical axis (the line where the load from the hip to the ankle passes through the knee) from an arthritic part of the knee to a healthy part. Tibial osteotomy is conventionally done for medial compartment OA (varus knee) and femoral osteotomy for lateral compartment OA (valgus knee).
Summary:
- Weight loss together with shifting load from the site of maximum damage is the most effective way of treating OA of the knee.
- Painkillers and NSAID may be required during this process to achieve objectives.
References
- https://www.jrheum.com/subscribers/04/70/22.html
Meniscus Tear

The function of the meniscus is to effectively make the flat surface of the tibia into a curve that matches the shape of the femur (see diagram A). When the meniscus is torn through an aging process the curved surface of the femur articulates on the flat surface of the tibia generating point loading (see diagram B) that leads to cartilage breakdown.
A: Intact Meniscus B: Torn Meniscus
A meniscus can also tear through injury. This is much rarer than a meniscus tearing through an ageing process. The injury that tears are meniscus is often part of a more complex injury pattern such as an associated ligament tear.
A small stable tear Close to the attachment of the meniscus to the knee can often go on to heal. An unstable tear especially if it has the configuration of a bucket handle tear (see diagram above) can block knee movements (“locked knee”). If this occurs surgery is normally necessary to “unlock“ the knee joint.
If the sufferer of a traumatic meniscus tear is young and a tear has occurred close to the outer rim of the meniscus it could be repaired depending on the pattern of the tear. Meniscus tears that occur through ageing is not suitable for repair as the tissue is weak through the ageing process.
Non-Surgical treatment for knee arthritis
Non-operative treatment for Knee Arthritis
Operative treatment for Knee Arthritis
Arthroplasty (knee replacement) surgery involves cutting out all or part of the knee joint and replacing it with a metal and plastic bearing
Osteotomy surgery invloves re-shaping the tibia or/and the femur. The altered shape allows for the forces of gravity to pass through the healthy part of the knee
References:
https://eor.bioscientifica.com/view/journals/eor/6/2/2058-5241.6.200102.xml
ICRS National Registry Data for your surgeon 2023:
https://acrobat.adobe.com/id/urn:aaid:sc:EU:b1502b99-306c-46a1-87ae-ce0860712428
Osteotomy around the Knee
Meaning:
Osteotomy noun: osteotomy; plural noun: osteotomies
The surgical cutting of a bone to change its shape and to allow for realignment of the leg. By changing the alignment of the leg, the surgeon can control where forces such as gravity passes through the knee joint. By changing how gravity passes through the knee joint the surgeon can treat conditions such as osteoarthritis and instabilities.
The mechanical axis has been moved from the arthritic part of the knee to the healthy part of the knee
X-ray a: demonstrates a mechanical axis (the force line between the centre of the hip and the centre of the knee). There is a mechanical axis deviation (MAD) to the outside of the knee joint. This patient is suffering from arthritis pain on the outside of the knee.
X-ray b: demonstrates a mechanical axis deviation to the centre and inside of the knee. This was achieved by removing a small wedge of bone from the inside of the femur.
Bone wedge added to the medial side of the tibia to treat, medial knee arthritis
What’s the difference between knee replacement and osteotomies surgery for arthritis?
Knee replacement involves removing half or all of the knee joint and replacing it with metal and plastic parts.
The choice between knee replacement and osteotomy.
|
|
Knee Replacement |
Osteotomy |
|
Very active patient |
Not recommended |
Recommended |
|
Sports |
Bowling, golf and social tennis |
Any sport including jumping and running |
|
Stage of arthritis |
End stage (Gr IV). Bone-on-bone |
Any stage of arthritis depending on pain |
|
Patient age |
Elderly, retired |
Any age, younger working |
|
Leg deformity |
Straight leg |
Severe bowing or knock-knees |
The factors in this table are not mutually exclusive and it requires the judgement of the surgeon and the choice of the patient before taking these factors into account before deciding on which is the most appropriate treatment for your arthritis.
The history of osteotomy in the treatment of arthritis and knee instabilities
Osteotomy has been used to treat meat conditions for longer than orthopaedic. Surgery has been a recognised branch of medicine. The word orthopaedic is a combination of the Greek words for healing (paedic) and ortho (to make straight).
Hippocrates (c. 460 – c. 370 BC) published images of a device he used to straighten legs, so we can consider that clinical osteotomy goes back in time to at least to his era.
John Rhae Barton (1794 - 1871) was an American Orthopaedic Surgeon. Considered the pioneer of modern osteotomy surgery.
William MacEwen (1848 - 1924) treated children's deformities, a lot of which were caused by poverty and poor nutrition (Ricketts disease for example).
He was born on the Isle of Bute and worked in Glasgow (Scotland)
What is the place of Osteotomy Surgery in the 21st Century?
Osteotomy of the lower femur and/or upper tibia is a safe and reliable surgical treatment for:
- Osteoarthritis of the knee in young or active patients.
- Severe knee instabilities that cannot be fixed with ligament reconstructions. its own. It is also used for ligament reconstruction is that have failed due to malalignment of the joint or bones that have sub-optimal shape for stability.
Advantages of Osteotomy
Osteotomy relieves pain and preserves the natural knee joint, delaying the need for a knee replacement for some years. It can allow a younger patient to lead an active lifestyle. Following recovery, the patient is permitted to return to all activities, even impact sports.
As time passes, arthritis in any knee will progress. The joint will then still be suitable for replacement surgery.
What does the surgery involve?
Long leg alignment x-rays to help your surgeon plan surgery accurately. An MRI scan is also required to ensure that there are healthy parts of the knee to move the load to.
During the operation accurate surgical cuts are made in either the tibia (shin bone) or femur (thigh bone) and occasionally both to achieve the planned correction of your leg alignment. The corrected bone is held firmly in place with a metal plate and screws.
Arthritis on the medial side of the left knee in a 38-year-old ex-professional athlete
Possible Complications of Osteotomy around the Knee
The most common complications are:
- Any major surgery involving general anaesthesia poses a low risk of strokes, heart attacks, pneumonia, and blood clots. Blood clots, or deep vein thrombosis (DVT), are complications of knee osteotomy or knee replacement, but only affect a small percentage of patients. It is standard for patients to receive blood thinning medication following osteotomy surgery.
- The surgical area can become infected. If the infection does not respond to antibiotics, another surgery or series of surgeries may be required.
- The nerves or blood vessels that runs down the back of the leg can be damaged during surgery.
- Compartment syndrome is when muscle compartments swell abnormally after surgery and require an emergency operation to release them.
- The bones at the osteotomy site may fail to grow together and heal this is often but not always due to infection that may require further surgery and a long course of antibiotics in your veins to control.
- Under-correction (wedge of bone that is removed or added in is too small) can result in incomplete pain relief.
- Over-correction can result if the wedge of bone added or taken away is too big. This means a knock-kneed person would become bowlegged or vice-versa.
- Because a wedge of bone has been added or taken away, a patient’s legs may be different lengths after surgery.
- Hardware irritation (symptoms from the presence of the plates and screws) may require removal of the implant once the osteotomy has healed.
Before electing to have knee osteotomy surgery, patients should talk to their surgeon about the potential risks and complications.
Returning to work
Return to work depends on your job. If you have a desk-based job, you can return to work when your pain allows, and you can travel to work safely. This can take up to six weeks. If you have a job that involves heavy lifting, or moving objects, you are likely to need a longer recovery period of up to 3 months.
Driving
You may return to driving when you have safe control of your car, this can take up to 6 weeks but usually much sooner.
UKKOR Data for your surgeon 2023
https://acrobat.adobe.com/id/urn:aaid:sc:EU:fa2d2bcb-e37f-4e6e-9dc1-31efc0e6e8a6
ACL Rupture
Knee swelling due to bleeding inside the joint
MRI appearance of ACL Rupture
Early Treatment
Early Full Knee Extension
Surgery for ACL Tears
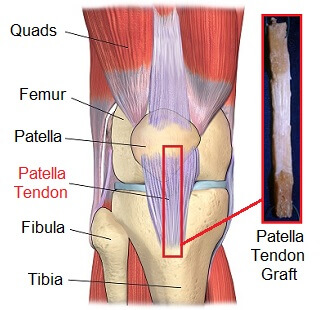
Tissue from your own body
- Hamstring tendons
- Patella bone-tendon-bone

Rehabilitation

What Are the Results of my ACL Reconstruction Surgery?
NLR is the acronym for National Ligament Registry
This is a database where all regular ACL Reconstruction Surgeons collect the data of patients (symptoms and disability), the surgery performed and the outcome of surgery.
NLR data for your surgeon 2023:
https://acrobat.adobe.com/id/urn:aaid:sc:EU:db758a9f-5bdc-440f-bc69-4043887fbf34
Patella instability
Patella instability means an unstable knee cap. It occurs when the patella (kneecap) moves out of the groove at the end of the thigh bone (femur) that holds it in place.
When you bend and straighten your knee the kneecap moves up and down in the groove that has the shape of the inside of the keel of both. The groove is called the trochlea groove. With patella instability the kneecap does not track in the groove the way it should. It might jump to the side and dislocate (completely come out of the socket) or it might just slightly over the edge of the groove and return immediately and this movement is called subluxation.
Conditions that contribute to patella instability


 Previous traumatic dislocation of the patella. This usually involves a very severe twisting injury with or without direct contact that causes the patella to sit on the outside of the knee. This is a very painful condition and sometimes requires attendance to A&E department to get the patella relocated to the front of the femur.
Previous traumatic dislocation of the patella. This usually involves a very severe twisting injury with or without direct contact that causes the patella to sit on the outside of the knee. This is a very painful condition and sometimes requires attendance to A&E department to get the patella relocated to the front of the femur.- Generalised ligamentous laxity: A condition way you genetically inherited ligaments that have more elastic property than they should. Such very stretchy ligaments may cause the kneecap to dislocate with very little or no force. Usually this is less painful as the kneecap can very easily slope in and out of the socket.
- Trochlear dysplasia: With the groove on the front of your femur that the kneecap runs in is particularly shallow or even convex.
- Genu valgum (knock knees) this condition will make the quadriceps full your kneecap in 1 direction and the kneecaps attachment to the tibia (shin bone) in another direction ideally this should be in equal and opposite pull in a straight line. Because there is an ankle there will also be a force vector in the lateral (outside) direction pulling the kneecap to a dislocated/subluxed position.
- Malrotation of the femur and/or the tibia relative to each other causing the kneecap to be pulled towards the lateral (outside) direction.
Symptoms of patella instability
- Or knee buckles for no apparent reason and struggles to support her weight.
- The patellar slipped off to the side.
- The knee catches during movement.
- pain at the front of the knee that increases with activity.
- Pain that is often worse with going or downstairs. Pain when sitting, especially in confined spaces such is in the back of a car.
- Knee stiffness often after sitting for a short period.
- Uncomfortable swelling and pain that improves when you stand up and walk around after a period of sitting
Treatment for patella instability
Nonoperative treatment:
This should always be the line of management in newly diagnosed cases. Unless there is very obvious cartilage damage on the patella or the front of the femur surgery is not necessary as a first-line measure. Nonoperative treatment is usually in the form of physiotherapy and home strengthening programme. This strengthening programme should involve not just the quadriceps but also the hamstrings and the pelvic stabilising muscles. The physiotherapist should achieve to get the balance between these groups of muscles. This is called enhancing lower limb proprioception.
You may be surprised how weak your progress section is in knee with an unstable patella. A good test this just try and stand on 1 leg. If he can achieve this try and stand on 1 leg with your eyes closed. If with you exercise programme you can eventually achieve this try and stand on 1 leg with your eyes closed while you are brushing your teeth. If you repeat this routine on a regular basis, you may find that your patella instability symptoms improve if they are of a mild nature.
Other nonoperative treatments that your physiotherapist may imply for temporary relief might be a local pressure garment or typing. This however might be counterproductive if used for prolonged periods of time as muscle strengthening and balance will be inhibited.
Operative treatment:
If nonoperative measures have failed to control your symptoms and your symptoms have become more than just a nuisance consideration might be given to operative treatment of your knee. Operative treatment of course always come with associated risks. These risks may be rare for minor you have to ensure that you will be able to live with them or alternatively go through additional treatment to get rid of them should that occur.
Operative treatment is normally used as a first-line treatment if your patella instability or kneecap dislocation has resulted in cartilage damage to your knee. There may be a loose body or a defect and the articular cartilage surface of your knee. Depending on several factors your surgeon will decide whether to treat the cartilage defect on its own or preferably with a procedure that will stabilise your patella to prevent further dislocations.
Before the type of surgical procedure can be chosen your surgeon will normally do further tests (in addition to an MRI scan) to define any contributing factors to your patella instability. These will normally involves looking at the alignment of your legs when standing. It will also involve looking at x-rays that of your leg from the side to be able to judge the height of the patella and the depth of the trochlea groove. Your surgeon might also choose to perform a CT rotational profile (this is rarely done as a first-line investigation). It will be to look for any rotational problems contributing to your patella instability.
The type of surgical procedures used to stabilise your patella can be categorised into:
- Soft tissue procedures and
- Bony procedures.
Soft tissue procedures will normally be to either repair or reconstruct a torn or deficient (stretched) medial patellar femoral ligament (MPFL).
Bony procedures may involve:
Changing where the patella tendon attached is to the tibia to bring it in line with your quadriceps pull. This surgery is called tibial tuberosity transfer (TTT).
Correcting alignment of your leg. If you suffer from knock knees this will bring the femur in line with the patella and the tibia to ensure that the femur, patella and tibia line up. This surgery is called osteotomy. It might be performed on the femur or tibia. It usually involves removing a small wedge of bone and then fixing the femur or tibia until it is healed.

Risks of surgery
Risks of soft tissue patella instability surgery:
- Numb patches on the skin around your knee or in the front of your shin. Even if this does occur you are only aware of it temporarily most of the time. It does not interfere with function and is usually due to disturbance of superficial skin nerves during surgery or in the healing post-surgery.
- Stiffness. This is a very rare complication of this particular type of knee surgery. It might involve scar tissue that has formed in or around her knee that restricts movement. It occasionally benefits from further remedial surgery. Remedial surgery is almost always delayed as the scar tissue can recur this sooner remedial surgery is performed after the index procedure.
- Infection. This is an exceedingly rare complication following this type of surgery. Usually, an antibiotic is administered minutes before surgery takes place.
- Deep vein thrombosis (DVT). This is also extremely rare complication. It is rare because patients are normally up and about on the feet on the same day as surgery. The surgery also usually takes place in less than an hour and overall soft tissue disturbance should be minor. Anticoagulants (anti-clotting agents) on normally only prescribed if you have specific risk factors such as being obese, having a family history of thrombosis problems, history of inflammatory bowel conditions or using certain types of oral contraceptive therapy. Please make sure that your alert your medical team if you believe that your along to 1 of these categories.
- COVID-19 related risks. We do not know the full effect the COVID infection might have on the results of surgery. We include do not know what effect surgery might have on subsequently contracting COVID 19. A lot has become clearer in research over the past months and years. What we do know is that contracting COVID after surgery might result in a more severe form of COVID should you have conditions that would normally give you a more severe form of COVID such as smoking, obesity, serious heart lung or kidney conditions. Your level of COVID severity might also be aggravated in certain types of very major surgery where the body's immune system is severely challenged at the time of the contracting COVID. Within national vaccination programme at present COVID related risks are becoming much less of a concern in surgery that results in minimal tissue damage and wear a return to mobility normally occurs within hours or days.
Risks of bony procedures for patella instability:
- Over/under correction. Meticulous pre-surgical planning with the use of state-of-the-art software normally mitigates against this. Despite this however, correction may end up being more or less than planned. Very rarely is remedial surgery required.
- Loss of correction. There may be movement at the osteotomy site following surgery. This could be from failure of the internal fixation to control the new shape of the bone, or it might be due to factors such as weak bone or delayed healing.
- Hardware irritation. Rest occasionally requires the internal fixation used to stabilise the osteotomy or tibial tuberosity transfer to be removed. The surgery is normally very minor. You could normally take full weight and resume full activities that you up to removal of the hardware without any restrictions.
- Hardware malfunction or failure. This too is a very rare complication. If there is movement at the osteotomy site it may cause the internal fixation to break through fatigue failure. Usually this is associated with pain when using the leg.
- Infection. He this is a rare complication. Normally antibiotics are administered both before and after surgery. If you have any potential source of infection such as red or bleeding gums, mouth ulcer, ingrown or painful toenails, inflammatory bowel conditions such as diverticulosis or diarrhoea at the time of surgery please inform your medical team as soon as possible. Any of these could result in bacteria entering your bloodstream that will cause an infection at the site of the osteotomy. If these bacteria attached themselves to the metal used full stabilising your osteotomy where they will become invisible to your body's immune system. This results in a slow grumbling infection preventing the bone from healing. Under these conditions you may require the exchange of internal fixation, bone graft and prolonged treatment with antibiotics through your veins.
- Failure of the bone to heal. Occasionally this may be due to coexisting low-grade infection. If thought to be present, he may require a CT scan for the diagnosis. This may then be followed with further surgery to get the bone to heal.
- Deep vein thrombosis. Please see soft tissue patella instability procedures.
- Nerve or blood vessel injury. This is a very rare complication. During most osteotomy procedures the nerves and blood vessels are not routinely visualised during the surgical procedure. Nerve and blood vessel protectors on normally placed before any bone surgery is undertaken. Extremely rare conditions however there might be up normal anatomy or conditions that tender or bind the nerve or blood vessel to the site of bone surgery.
- Numb patches. Please see under risks for soft tissue patella instability procedures
- COVID-19 related risks. Please see under risks for soft tissue patella instability procedures
Ankle Instability
Chronic ankle instability is a condition characterized by a recurring giving way of the outer (lateral) side of the ankle. This condition often develops after repeated ankle sprains. Usually, the giving way occurs while walking or doing other activities especially on uneven surfaces. Many athletes, as well sedentary individuals, suffer from chronic ankle instability.
People with chronic ankle instability often complain of:
- A repeated turning of the ankle, especially on uneven surfaces or when participating in sports
- Persistent discomfort and swelling
- Pain or tenderness
- The ankle feeling wobbly or unstable
Causes
Chronic ankle instability usually develops following an ankle sprain that has not adequately healed or was not rehabilitated completely. When you sprain your ankle, the ligaments are stretched or torn. The ability to balance is affected. Rehabilitation is needed to strengthen the muscles around the ankle and retrain the tissues within the ankle that affect balance. Failure to do so may result in repeated ankle sprains.
Repeated ankle sprains often cause chronic ankle instability. Each subsequent sprain leads to further or stretching of the ligaments, resulting in greater instability and the likelihood of developing additional problems in the ankle.
Diagnosis
In assessing, the surgeon will ask you about any previous ankle injuries. The surgeon will examine your ankle to check for tender areas, signs of swelling and instability of your ankle. X-rays or other imaging studies may be helpful in further evaluating the ankle.
Nonsurgical Treatment
Treatment for chronic ankle instability is based on the results of the examination and tests, as well as on your level of activity.
Nonsurgical treatment may include:
- Physiotherapy. Physical therapy involves various treatments and exercises to strengthen the ankle, improve balance and range of motion and retrain your muscles. In later rehabilitation, you will receive training that relates specifically to your activities or sport.
Bracing. Some patients wear an ankle brace to gain support for the ankle and keep the ankle from turning.
- Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be prescribed to reduce pain and inflammation.
When Is Surgery Needed?
In some cases, the surgeon will recommend surgery based on the degree of instability or lack of response to nonsurgical treatment. Surgery usually involves repair or reconstruction of the damaged ligament(s). The surgeon will select the surgical procedure best suited for your case based on the severity of the instability and your activity level. The length of the recovery period will vary, depending on the procedure or procedures performed.



2 Weeks in POP then 4 weeks in AirCast (or equivalent) walker boot
After surgery
The ankle is usually placed in a below knee plaster cast. You may stay in hospital for that night. On discharge from hospital you will leave the hospital on crutches but taking some weight through the plaster cast.
After two weeks the plaster cast is removed. The sutures are removed and you are supplied with an Aircast boot. You will normally use the Aircast boot for approximately four weeks. You can usually take full weight through the ankle if the wound is satisfactory and in the absence of pain. If you feel a bit unsteady there is nothing wrong with continuing the use of the crutches.
Once you are mobile in the Aircast boot and the wound is satisfactory you can commence physiotherapy and range of motion exercises. It is important to bring the ankle up towards the direction of your head under its own power as well as with passive means. This may include the use of a small hand towel that is slung around the front of your foot while your knee is in the bent position.
Advice for the time in the walker boot
- Cover the surgical scars with a dry surgical dressing
- DO NOT have the liner of the boot in direct contact with your skin
- DO NOT use sauna's, jacuzzi's steam rooms or public swimming pools
- Shower once or twice a day without using detergents, ointments or creams on the surgical scar
- Dry the skin with kitchen roll and not your usual hand towel
- ONLY use the boot for walking. Remove it at all other times and allow the skin to air
Benefits of surgery
- Stable ankle.
- Return to sport.
Risks of surgery
- Numb patches on the skin of the foot and ankle adjacent to the scars.
- Wound infection. Please play close attention to the instructions that are given when the plaster cast is removed at two weeks. (Antibiotics are administered at the time of surgery to reduce this risk. )
- DVT (deep vein thrombosis). Most patients are commenced on a anticoagulation medication following surgery for a week or two depending on the other risk factors and risks of bleeding.
- Recurrent instability. This may be due to the posture of the foot and ankle or coexisting injuries.
- Ankle stiffness due to internal scar tissue formation.
Driving
You may return to driving when you are confident that you can control your vehicle. Please note: You must not drive with the Aircast boot in place. You will need to keep an ordinary driving shoe in your car to swap into before setting off.
Ankle pain is often due to an ankle sprain but can also be caused by ankle instability, arthritis, gout, tendonitis, fracture, nerve compression (tarsal tunnel syndrome), infection and poor structural alignment of the leg or foot. Ankle pain can be associated with swelling, stiffness, redness and warmth in the involved area. The pain is often described as an intense dull ache that occurs upon weightbearing and ankle motion.
Initial treatment may consist of rest, ice, elevation and immobilization but may also include nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, physiotherapy and corticosteroid injection. A surgeon can best determine the cause of the ankle pain and appropriate treatment options after a consultation, examination and an MRI scan with or without an x-ray of the ankle. Occasionally in arthritic conditions weight-bearing x-rays of the ankle and leg need to be obtained to see how the ankle behaves and a load.
For more information on ankle pain, see these topics below:
- Achilles Tendinopathy
- Ankle Arthritis (Osteoarthritis)
- Gout
- Peroneal Tendon Injuries
- Posterior Tibialis Tendon Dysfunction
- Talar Dome Cartilage and Bone Lesions
- Tarsal Tunnel Syndrome (Nerve Compression)
Achilles Tendinopathy/Disorders
The Achilles tendon is a band of tissue that connects a muscle to a bone. It runs down the back of the lower leg and connects the calf muscle to the heel bone. Also called the heel cord, the achilles tendon facilitates walking by helping to raise the heel off the ground.
Achilles tendinopathy A common disorder that occur in the heel cord is achilles tendinopathy. It is characterised by alternating episodes of tendon breakdown and inflammation. Tendon breakdown occurs when the tendon loses its organized structure and develops microscopic tears. Sometimes the degeneration involves the site where the achilles tendon attaches to the heel bone but mostly it occurs between five and 7 cm from its insertion to the heel bone. In rare cases, chronic degeneration with or without pain may result in rupture of the tendon.
Causes It is usually caused by a sudden increase of a repetitive activity involving the Achilles tendon. Such activity puts too much stress on the tendon too quickly, leading to micro-injury of the tendon fibres. Due to this ongoing stress on the tendon, the body is unable to repair the injured tissue. In its attempt to heal the injured tissue the body produces an inflammatory reaction to bring in cells that normally repair and heal. The structure of the tendon is then altered, resulting in repetitive inflammation episodes with the resulting pain.
At risk groups
- Athletes are at high risk for developing disorders of the Achilles tendon.
- Achilles tendinopathy also common in individuals whose work puts stress on their ankles and feet, such as laborers, as well as in “weekend warriors”—those who are less conditioned and participate in athletics only on weekends or infrequently.
- People with excessive pronation (flattening of the arch) have a tendency to develop achilles tendinopathy due to the greater demands placed on the tendon when walking. If these individuals wear shoes without adequate stability, their overpronation could further aggravate the Achilles tendon.
Symptoms
- Pain—aching, stiffness, soreness or tenderness—within the tendon. This may occur anywhere along the tendon’s path, beginning with the tendon’s attachment directly above the heel upward to the region just below the calf muscle. Pain often appears upon arising in the morning or after periods of rest, then improves somewhat with motion but later worsens with increased activity.
- Tenderness, or sometimes intense pain, when the sides of the tendon are squeezed. There is less tenderness, however, when pressing directly on the back of the tendon.
- When the disorder progresses to degeneration, the tendon may become enlarged and may develop nodules in the area where the tissue is damaged.
Diagnosis In diagnosing achilles tendinopathy, the surgeon will examine the patient’s foot and ankle and evaluate the range of motion and condition of the tendon. The extent of the condition can be further assessed with ultrasound and magnetic resonance imaging (MRI).
Treatment: Treatment approaches for achilles tendinopathy are selected on the basis of how long the injury has been present and the degree of damage to the tendon. In the early stage, when there is sudden (acute) inflammation, one or more of the following options may be recommended:
- Immobilization may involve the use of a cast or removable walking boot to reduce forces through the Achilles tendon and promote healing.
- To reduce swelling due to inflammation, apply a bag of ice over a thin towel to the affected area for 20 minutes of four or five times a day. Do not put ice directly against the skin.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be helpful in reducing the pain and inflammation in the early stage of the condition.
- Orthotics for those with overpronation or gait abnormalities, custom orthotic devices may be prescribed.
- Night splints help to maintain a stretch in the Achilles tendon during sleep.
- Physiotherapy. This may include strengthening exercises, soft-tissue massage/mobilization, gait and running re-education, stretching and ultrasound therapy.
- Low frequency shockwave therapy. Where a wave of sound is focused on the degenerative tissue to break up scar tissue and encourage a healing response internally.
- High-volume injections. This is where saline (salt water) with local anaesthetic is injected in the interval between the Achilles and the surrounding membrane to stretch the membrane or paratenon (that is often the source of pain) away from the tendon. This procedure is done under ultrasound control by a qualified radiologist.
Surgery: If nonsurgical approaches fail to restore the tendon to its normal condition, surgery may be appropriate. The surgeon will select the best procedure for the damaged and degenerative parts of the tendon, based on the extent of the injury, the patient’s age and activity level.
Prevention: To prevent Achilles tendinopathy from recurring after surgical or nonsurgical treatment, the surgeon may recommend strengthening and stretching of the calf muscles through daily exercises. Wearing proper shoes for the foot type and activity is also important in preventing recurrence of the condition.
In which Hospital will my operation take place?
- BMI Woodlands Hospital
Morton Park
Darlington, Co. Durham
DL1 4PL
01325 341700 - Tees Nuffield Health
Junction Road
Stockton on Tees
TS20 1PX
01642 360100 - Friarage Hospital
Northallerton
North Yorkshire
DL6 1JG
01609 763110
Our patients under the age of 16 are required to be treated in a Hospital licensed for paediatric surgical services. The only Hospital in this area suitable for this purpose is the Friarage Hospital in Northallerton where limited theatre availability for our patients under the age of 16 exists. Flexibility will therefore be needed to finalise an operation date.
How do I get my operation authorised by my Insurance Company?
After your consultation to arrange treatment you will need to contact your Insurance Company to inform them of:
- Operation Code(s)
- The Hospital
- The Length of Hospital Stay
This information will be given to you by your Consultant when you discuss your treatment plan in the outpatient department.
What time will my operation take place?
If you phone the hospital where your operation will take place on the day prior to your proposed surgery they can normally give you an indication if your operation will take place in the morning or in the afternoon. We cannot however be any more specific than that because the final order of the operating list can be subject to last minute changes due to medical conditions in some patients, instrument availability and the availability of other essential services such as radiography and theatre. If your operation is in the morning the nursing staff can give you a reasonable accurate estimate of your theatre time by 9 am and 2 pm if your operation is in the afternoon.
What is the patient’s responsibility for the day of surgery?
Do not eat or drink anything after midnight if your operation is set to take place in the morning or if the time of your surgery is not decided yet. You can have a light breakfast prior to 0730 hrs if your operation is definitely scheduled for the afternoon.
You will need to be dropped off and picked up after your operation. You will not be able to drive yourself for at least forty-eight hours after completion of your operation (see exceptions under “when can I drive after my operation”).
If you are on regular medication you can take these with a small amount of clear fluid first thing in the morning. Please note medication such as Warfarin, aspirin and anti-inflammatories need to be discontinued for week or more prior to your surgery. If you are in any doubt please discuss these with the Pre-Assessment Team prior to your admission.
What is Pre-Assessment?
Pre-admission assessment is to ensure that:
- You do not have medical conditions that would make the proposed surgery or anaesthesia dangerous to you.
- Any medical condition that you may be suffering from is under control.
- Any tests that may be required by your Anaesthetist are completed prior to your admission.
- To answer any questions you may have related to your stay in the Hospital.
- To ensure that you are not a carrier of infections such as MRSA.
What if I Travel from Abroad for my Operation or Need to Use Air Travel to get to / from my Operation?
Please liaise closely with the CSIS office by phone / e-mail well in advance. We can make suggestions on the timing of your flights as well as suggestions for accommodation and transport links. On leaving the Hospital you will need a letter to state that you are fit to fly. You will also need medication to prevent deep vein thrombosis (DVT) if your flight is within two weeks of surgery.
Dressings and Plaster Casts:
Nursing Staff on the Ward will give you detailed advice on dressings and advice if you are in a Plaster of Paris cast. They will inform you of the arrangements for removal of your sutures and attendance at the plaster room for removal of exchange of plaster cast. If you have any concern about your dressings or operation site please phone the Hospital where your treatment took place. Frequently telephone advice only is required. If this is not satisfactory you may have to attend the Hospital in question for the RMO (Resident Medical Officer) to examine you.
Mobility:
Depending on the type of operation that you have undergone you may be required to use crutches or a brace when you go home. The Hospital Physiotherapists will make sure that you are fully mobile including the use of stairs before you go home.
Most operations performed by your consultant have postoperative rehabilitation protocols that have been written by Mr van Niekerk with advice from his physiotherapy and rehabilitation medicine colleagues. It is therefore strongly recommended that you remain under the supervision of a suitably qualified physiotherapist at least until you see your consultant for the first postoperative visit that would normally take place 4-6 weeks after your operation.
Post operative protocols (See Health Professional Page) are to outline minimum (not ideal) targets to achieve. The guidelines are adapted by surgeon and physiotherapist based on age, lesion site and size, stability and alignment of the leg and response to protected weight bearing in the first 2-3 weeks.
Physiotherapy:
After your operation the Hospital Physiotherapists will give you advice on mobility, precautions and exercises for the next week or two. After this period your Consultant will want you to undergo the treatment and supervision of Outpatient Physiotherapist. Please make sure that you arrange this to commence a week or at most two, after your operation. If you already have a physiotherapist please make sure that you inform CSIS by phone / e-mail so that relevant correspondence can be sent to our physiotherapist prior to your attendance after your operation. If you do not have an outpatient physiotherapist please contact CSIS by phone / e-mail prior to your operation to enable use to recommend a physiotherapist who is easily accessible to you and registered with your insurance company and most of all has experience in the rehabilitation of your particular type of operation.
Further Outpatient Attendance:
You will be contact by post within a week of your operation to arrange a time and date as well as a venue for a follow-up appointment with your Consultant. If the time, date or venue is not convenient please e-mail CSIS with your availability.
When can I drive after my operation?
The responsibility to decide when to return to driving after an operation is entirely yours. We do not recommend that you drive at all for two days after any operation. It may be possible to return to driving after forty-eight hours if your operation was on your left knee / ankle. That is to say that if your knee or ankle is not restricted by dressings, a brace or a plaster cast.
If you had any surgery to your right knee / ankle then you should discuss to return to driving with your physiotherapist or Consultant. The general advice would be that your right knee / ankle should be free from dressings, braces or any other restriction and that you are confident that you can perform an emergency stop and be in full control of your motor vehicle.
- Stay well hydrated
- Make sure you do calf exercises in-flight.
- Ensure that you get up and move about every 20 minutes.
- If you have no contra indications then a half of an aspirin (150 mg) will also reduce your risk of DVT. This can be commenced any time now and continued for three weeks following air travel.
National surgical registries are databases for very specific orthopaedic operations. The registries record patient symptoms before and after the operation. It allows for surgeons to enter verifiable information such as biomechanical measurements based on x-rays and data on the specific operation performed on each patient. It also allows for patients and surgeons to record complications.
National registries are used by the NHS and private medical insurers to assess the value of an operation based on the outcomes. Values such as EQ-5D measures five dimensions quality of life in health terms that include mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.
It allows patients to match their expectations of the operation to what can be achieved. It also helps surgeons to look at large groups of patients and going similar treatment and making improvements in surgical technique as well as pre-and post surgical care. It benchmarks individual surgeons against national average outcomes for the particular operation.
Below is a link that summarises the caseload and outcomes of your surgeon as benchmarked against national averages. It includes data from the UK Knee Osteotomy Register (UKKOR), the National Ligament Registry (NLR), and the International Cartilage Repair Society Register (ICRS).
https://acrobat.adobe.com/id/urn:aaid:sc:EU:d7b1088c-e49d-4d24-bcba-5844c52a9b94
